A Transition from the Early to the Modern Era of CVD Epidemiology: ‘The Pause,’ 1968 to 1972
It is difficult to imagine today the intensity, vigor, and great expectations of the field of cardiovascular disease epidemiology and prevention in the fall of 1968. First-phase prospective epidemiologic evidence was in. Findings on follow-up experience for risk factors of diet, serum cholesterol, blood pressure, tobacco, and physical activity were mostly strong, consistent, independent, graded, and universal, and were largely congruent with plausible mechanisms; pathways were demonstrated in the clinic and laboratory. Causal inference was strong. Prevention through risk factor modification was theoretically likely. The risk factor paradigm for atherosclerotic disease and heart attack had replaced that of the ineluctable result of aging.
Nevertheless, the two major initiatives of the day toward experimental tests of the risk factor hypothesis, that is, the National Diet-Heart Trial, and ‘Jumbo,’ the first proposal to NIH for a multiple-risk-factor trial, were at that moment dying on the twin barricades of academic resistance and overwhelming cost. Policy was in pause and paradox. Government-establishment support was absent both for the broad recommendations of the prevention activists and for the only rational alternative: “definitive” experiments as preventive trials. NIH was in virtual paralysis, panicked over the prospect of massive, costly trials usurping all its newly gained cardiovascular program and resources. The U.S. Congress had not yet got the message of the potential for prevention and the costly but good investment that science offered.
It was then that a few clear heads began to focus, lay out the evidence, and propose a multiple strategy that could be used to carry the day for prevention. The strategy came together powerfully in a planning conference held at Makarska on the dramatic Adriatic coast of Yugoslavia in fall 1968.
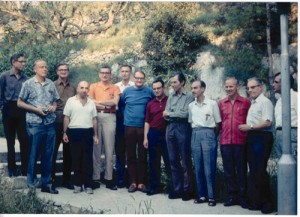
Participants in the Makarska Conference on Mass Field Trials in the Prevention of Coronary Heart Disease, Makarska, Yugoslavia, September 19-24, 1968 are portrayed left to right: Henry Taylor, Thomas Chalmers, Austin Heady, Jerry Stamler, Richard Remington, Samuel Fox, Gosta Tibblin, Igor Glasunov, Geoffrey Rose, Frederick Epstein, Marti Karvonen, Ancel Keys, and Jerome Green. Not pictured but taking the photo: Henry Blackburn.
It is a problem to separate the designers from the architects from the contractors, builders, and workers in what was to become a great leap forward for cardiovascular prevention that took place in the next period. But agencies representing all of these societal elements either came or sent their delegates to Makarska that September. They assembled in that unusual place because the ‘ole boys club,’ the Keys and White research committee, by then the officially designated Scientific Council on Epidemiology and Prevention of the International Society and Foundation of Cardiology (ISFC), had cajoled cardiovascular leaders internationally, raised interest, and scrambled to fund their participation, much of it out-of-pocket.
They also brought new movers on board, including the prevention guru and gadfly, Jeremiah Stamler, along with Geoffrey Rose, Richard Remington, Fred Epstein, Henry Taylor and eager others. Together with the wider community and key agencies, representatives were on board from the policy makers of the National Institutes of Health, the American Heart Association, World Health Organization, the London School of Hygiene and the U.S. Joint Commission on Heart Disease Resources; all assembled in Makarska.
The upcoming bright-eyed generation of young CVD epidemiologists was also there, either as members of the Seven Countries Study 10-year survey team, or as fellows or faculty for the first 10-day Seminar in Cardiovascular Disease Epidemiology. This seminar, the first international training effort of CVD epidemiology, was sponsored by the ISFC and proved a happy add-on to the intellectual feast that was Makarska that fall.
Makarska Recommendations
After summarizing the evidence and the possibilities for prevention, the Makarska conferees proposed a series of specific initiatives and a framework for action. All of the agencies were to depart for home and develop seminal policies and programs for CVD prevention in the ensuing years, in particular, the 1970 Report of the U.S. Joint Commission on Heart Disease Resources; the 1971 National Heart and Lung Institute Task Force on Arteriosclerosis, and a series of WHO Expert Reports on Preventive Trials and Community Prevention strategies.
The savvy delegates focused on the chief issue at hand, proof acceptable to skeptics of the clinical and laboratory science community who still were not buying into preventive practice or population strategies of CVD prevention.
The Conference summary, quoted fully here for its historical place, unequivocally recommends explicit studies and single and multiple risk factor preventive trials:
Since WWII, tremendous research advances have been made in clarifying the pathogenesis and etiology of atherosclerotic disease. In particular, extensive new findings have been assessed indicating the role of mode of life (particularly habits of eating, smoking, and sedentary living) and the elevated risk factors causing the epidemic of premature clinical coronary disease in the developed countries.
This new knowledge — available in its essential features by the late 1950s — points to the possibility of an historic breakthrough: the large-scale prevention for the first time in human history of a major chronic non-infectious disease. [A series of] “first generation” trials have accrued valuable, positive experience on the feasibility of such long-term studies. They have also yielded suggestive — but not conclusive — evidence that both primary and secondary prevention of clinical coronary heart disease can be achieved by dietary means.
Based on this knowledge and experience, medical research is in a scientific position to proceed rapidly and effectively to develop a series of “second generation” mass field trials on coronary prevention. These studies could be calculated to yield definitive answers within a decade concerning ability to bring the episode of premature coronary heart disease under control by widespread application of available research knowledge. They could explore a variety of approaches indicated by the research findings — for example, diet, exercise, cessation of cigarette smoking, drugs to correct hypertension, hyperlipidemia, hyperglycemia, hyperuricemia — singly or in combination. They could be developed on a national and international scale with extensive cooperation among competent, dedicated research groups in several countries, with an effective division of labor and with assurance of a high degree of scientific standardization and comparability.
… The task lies ahead of completing definitive protocols, assembling cooperative research groups, identifying populations for study, and beginning the actual trials.
In this connection, the Makarska Conference recognized that priority decisions were essential. Although — as this report indicates — the potential need exists for many types of trials, the complexity of duration, manpower demands, and costs of such studies, compels selectivity in implementation. For reasons noted in the previous section, the Conference emphasized the importance of giving highest priority to field trials aimed at assessing ability to achieve primary prevention by concurrently altering habits of eating, cigarette smoking, and sedentary living estimated to be at the root of the current epidemic of premature CHD. At the same time, the Conference urged that multiple studies be encouraged, since no single study can give definitive answers to the complex questions on coronary prevention confronting the community.
The Conference also took pains to emphasize the fact that little or no further significant scientific knowledge on coronary prevention is likely to be forthcoming without large scale, well-designed, well-controlled, and well-organized mass field trials. At this juncture, their accomplishment does not depend primarily on initiatives by concerned investigators or their organizations. The scientists are ready to proceed. The next steps are possible now, only if appropriate action is forthcoming from the key policy-making and grant supporting organizations, particularly governments. They must make the decisions and commitments concerning the funds necessary for the scientists to proceed with the work.
The Makarska message took hold; the planners dispersed to prepare worldwide a set of formal reports and to develop a generation of new studies and trials that initiated the Modern Era of CVD epidemiology and prevention. Makarska was quickly followed by the all-embracing, dramatic medical and societal recommendations of the Joint Commission on Heart Disease Resources Report in 1970. The commission report on atherosclerosis, chaired by Jeremiah Stamler, provided a framework on which the 1971 Task Force on Arteriosclerosis of the National Heart and Lung Institute could build its three-part research plan of clinical, laboratory, and population investigations (National Heart and Lung Institute Task Force on Arteriosclerosis 1971).
By 1972, that balanced strategy was fully conceived, funded, and organizationally structured, when the NHLI launched major prevention policy and issued requests for proposals for preventive trials: the community-based Hypertension Detection and Follow-up Program (HDFP). Lipid Research Centers (LRC), with population observations and lipid-lowering trials in contrasting populations, the Multiple Risk Factor Intervention Trial (MRFIT) of primary prevention in high risk men, and several secondary prevention trials among CVD patients.
In the same period, WHO coordinated British and European components of a Multiple Risk Factor Trial in Industry, while other active foci of preventive research moved forward in the UK, in Scandinavia, and on the Continent.
The full-blown U.S. policy was at long last presented, explained, and promulgated by Theodore Cooper, Director of the U.S. National Heart and Lung Institute, at the fall 1971 Scientific Sessions of the AHA.
Theodore Cooper Outlines a Giant Leap in U.S. CVD Research Policy, 1971-72
In fall 1971, after the long, simmering pause during which there was absent national research policy on the nation’s greatest killer, cardiovascular disease, the pot came to a boil. Ted Cooper, NHI Director-chef, cooked up a full mess of policy and served it in the Lyman Duff Lecture at the annual meeting of AHA (Cooper 1972).
At first hemming and hawing with self-deprecatory humor, he eventually came to the point: “I believe . . . that the time is now imminent for the development of a national policy in arteriosclerosis” (Ibid., 434).
Cooper proposed a major change in how the NIH deals with the health and social problem of arteriosclerosis, coupling morphological research with clinical physiology and biochemistry, linking pathologic data with clinical laboratory data, and working across traditional boundaries of research disciplines.
The need for a national policy for research should depend, he opines, on: “the magnitude of the problem, the importance that the public attaches to the problem, and the scientific, social and necessarily political possibilities of significant change in the acquisition of new knowledge and the application of it” (Ibid.).
He then defines the magnitude of the problem and for the first time calls attention to a decline in the number of U.S. deaths from all cardiovascular-renal disease from 1940-1970, still indicating that heart disease has actually been the #1 killer in the United States since 1910.
He deals colorfully with public attitudes toward coronary disease: for example, that coronary death was an “appropriate” way to die, sudden and clean. But he chides professional attitudes that claim the situation is such a long way from a breakthrough that attention in the interim should be directed elsewhere, challenging that idea: “. . . it does not seem to me to be profitable to pit one disease against another” (Ibid., 436).
Arteriosclerosis, he maintains, should have “allocation of national resources determined on a simple, factual basis, namely, its magnitude and the high likelihood that something can be done about it” (Ibid., 437). These, the NHI director states, had been major determinants in the brand new Heart Institute Program in Arteriosclerosis.
Particularly important for the prevention community, Cooper endorses prevention as a prime objective, but not applied solely to so-called “premature disease,” the target on most tongues, so that CVD was the anticipated consequence of aging: “I am unwilling to view the appearance of disease after the age of 65 years as inevitable, and I believe in the present state of ignorance of aging processes to say that something is ‘inevitable’ is akin to describing etiology as ‘idiopathic’” (Ibid.).
Cooper emphasizes that the new policy derives (in music to the epidemiologist’s ear) from any- and everywhere, saying that, “These data and ideas can be found in test tubes, in experimental animals, in individual patients, and in populations” (Ibid., 438). The next breakthrough, he claims, might come from any discipline.
The new national policy for research in atherosclerosis has these undertakings outlined by the Heart Institute Director:
- Prevention should be a prime objective of a program in arteriosclerosis
- Progress in understanding and conquest of the disease lies in basic research, with new concepts and new data from each of the major medical research methodologies, clinical, laboratory, and epidemiological
- Coordinated systems or groups of scientists interested in working on arteriosclerosis (SCORS, or specialized centers of research)
- Major trials of lowering blood lipids in the prevention of arteriosclerotic vascular disease
- Measuring the prevalence and distribution of blood lipid abnormalities in the population
- A specific test of the lipid hypothesis in a large-scale trial in patients at high risk because of their lipid characteristics
- A trial to assess the role of blood pressure control on the prevention of myocardial infarction, to include the young, black, and female as well as the middle-aged white male
- A trial of multiple risk factor lowering
Cooper then makes the first official mention of a multiple risk factor trial, following on the Makarska Report, the Jumbo Trial proposal, and other guidelines brought so vigorously to his attention during The Pause: “It seemed reasonable to extrapolate the observations to practical prevention by advocating a program which includes the elimination of cigarette smoking along with the reduction of serum cholesterol and control of blood pressure” in which the study would not be to disclose mechanisms, but to test the prevention concept overall. Thus, it would be a test of the application of knowledge rather than a clinical trial or a test of a hypothesis. “It is my opinion that the study of the lipid factor, the study of the hypertension factor, and the test of the multiple risk factor concept can and should be done concurrently.”
In a final plea for national program he opines: “Children must learn to take care of their hearts as well as their teeth.”
Cooper, the newly formed statesman for CVD prevention, then closes with a diplomatic plea that health decisions not come just from a scientific elite: rather “we must take our plans to the people, for in the final analysis it is the people, and their representatives, who make the priority decisions upon which the dollars and the programs depend.”
The Pause had ended.
U.S. pioneers in CVD prevention and their scientific colleagues around the world, now had a policy going forward. Direction, projects, and funds were soon to follow.
It is uncertain whether Ted Cooper, who had taken the heat from prevention activists for some years, ever received the credit he deserved for facing up to the epidemic problem of ailing arteries and for moving U.S. policy off dead center. At any rate, with apologies for Americentrism, we signify this moment in history as the beginning of the Modern Era of CVD Epidemiology and Prevention. (Henry Blackburn)
References
National Heart and Lung Institute Task Force on Arteriosclerosis. 1971. Arteriosclerosis: A report. DHEW Publication No. (NIH) 72-137, vol. 1. Bethesda, MD: National Institutes of Health.
Cooper, Theodore. 1972. Arteriosclerosis: Policy, polity, and parity. Circulation 45: 433-40.